 In oncology, cancer immunotherapy represents the cutting edge of cancer treatment. Deemed a breakthrough technology by Science magazine in late 2013, the current year has seen immunotherapy — an approach to cancer treatment wherein the body’s own immune system is optimized for fighting cancer cells — go from a little-known treatment option to a treatment technology that Big Pharma is investing in heavily. Just this afternoon, a breaking news story from Reuters reports that Merck’s immuno-oncology drug pembrolizumab, an experimental treatment for melanoma, is going to be approved by the FDA well ahead of a late October deadline.
In oncology, cancer immunotherapy represents the cutting edge of cancer treatment. Deemed a breakthrough technology by Science magazine in late 2013, the current year has seen immunotherapy — an approach to cancer treatment wherein the body’s own immune system is optimized for fighting cancer cells — go from a little-known treatment option to a treatment technology that Big Pharma is investing in heavily. Just this afternoon, a breaking news story from Reuters reports that Merck’s immuno-oncology drug pembrolizumab, an experimental treatment for melanoma, is going to be approved by the FDA well ahead of a late October deadline.
For those in the lung cancer community, immunotherapeutics are also being tested on the disease, with a particular variety known as “checkpoint inhibitors” beginning to show promise in clinical settings. However, while early data reveals that checkpoint inhibitors may hold the key for advancing lung cancer treatment, there is still more to be learned about how they work and which other drugs they should be combined with.
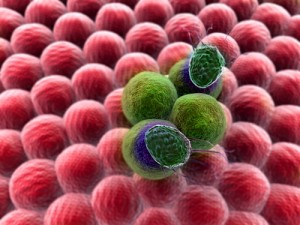
Checkpoint inhibitors are chemicals that disrupt the mechanism behind what allows tumors to disengage the body’s own T cells to fight cancer cells. When the inhibitor interacts with the right checkpoint, it can disable cancer’s ability to fool the immune system into leaving it alone, enabling a patient’s body to fight the disease like it would any other. To date, there have been many of these checkpoints identified by researchers, however, only two of them, PD-1/PD-L1 and CTLA-4, have been studied when using checkpoint inhibitors as an experimental therapy. While there are still many more to test, the good news is that the early, limited data reveals impressive results.
According to a recent article on Clinical Oncology News by Ted Bosworth, the data from these studies, which was recently on display at this year’s American Society of Clinical Oncology (ASCO) and summarized by Dr. Drew M. Pardoll, the cancer immunology director at Johns Hopkins University School of Medicine, revealed that the immunotherapeutic nivolumab, a monoclonal anti-PD1 antibody, markedly extended survival rates, with more than 20% of the patients treated with the drug still living two years after the study. The results were particularly stunning, since the participants were in the late stage of their disease at the time of the study and would not have been expected to live that long. The data also bore out evidence of anti tumor activity in about 20% of participants who were treated with single-agent checkpoint inhibitors.
Yet, in spite of the promising evidence, oncologists and researchers still believe that checkpoint inhibitors will have to be used in tandem with other dugs as a combination therapy in order to achieve optimal results. Pardoli pointed out that, while the 20% success rate was indeed impressive in previous studies, the fact that nearly 80% of participants had no meaningful response to checkpoint inhibitors means that the technology is still not understood well enough to be a one-size-fits all therapeutic solution for lung cancer. For researchers, the next step will be to determine if checkpoint inhibitors are paired best with other novel treatment options, such as cancer vaccines, anti-inflammatories, tyrosine kinase inhibitors, or other emerging therapeutic approaches.

